Read IKC’s Position Paper: Recommended Changes to Conditions for Coverage to Improve and Modernize Kidney Care
Kidney patients deserve better access to home dialysis.
Background
37,000,000 Americans are affected by kidney disease and 550,000 annually are on dialysis. However, the pathway to choosing where and how to do dialysis can sometimes be difficult for patients and their loved ones. Not all patients have access to the same choices for their dialysis care.
Self-dialysis, including peritoneal dialysis and home hemodialysis, is a safe and effective treatment option for patients facing permanent kidney failure—also known as End-Stage Renal Disease (ESRD) or End-Stage Kidney Disease (ESKD)—while they wait for a kidney transplant, or if they’re ineligible for a transplant.
Home dialysis offers logistical, economic, and quality of life benefits for patients experiencing kidney failure; but it’s widely underutilized in the United States despite the advantages it can offer.
The federal government and the kidney community agree that increased patient access to home dialysis is crucial. Nonetheless, existing federal regulations make it difficult or impossible for patients to access dialysis at home.
To give patients experiencing kidney failure the best chance at maintaining their quality of life, federal policies have to change to align with the goal of providing more patients the choice to receive their dialysis at home.
Our Mission
- Create a whole new paradigm that gives patients a choice in their dialysis.
- Empower kidney patients to access diverse innovations that improve their lives.
- Modernize existing policies and regulations to foster flexibility in patient care.
Our Positions
Medicare’s existing ESRD Conditions for Coverage apply a one-size-fits-all set of federal requirements for offering dialysis services whether patients are receiving dialysis in a clinic or treating at home. Yet, many of these requirements do not need to apply to self-dialysis options. Current regulations create unnecessary complexity and delays that prevent many patients from having choices in where and how they receive their dialysis.
Remove barriers that make it challenging for self-dialysis, home training, and support to be provided in existing health care settings.
Strengthen guidance to expand home dialysis training, support, and transitional care via in-center self-dialysis, with extra focus on marginalized communities.
Protect patient safety while giving providers more flexibility in skilled staffing to coach patients and care partners on independent skills-building, based on their own licensure or training.
Provide information to patients and the Centers for Medicare & Medicaid Services (CMS) on medical directors and owners of each dialysis facility.
Simplify and streamline requirements on what is needed to establish Medicare certification for a home training and support facility.
Expand options to provide accessible, safe virtual care, and training to patients electing self-dialysis modalities.
Winter 2022
Read Our Recommended Changes to Conditions for Coverage to Improve and Modernize Kidney Care
Patient Stories
 Gwenie lives on a ranch in a rural area of NE Montana. She is not new to the healthcare arena, but had no idea that she had CKD when she “crashed” into dialysis in Nov. 2020. With no major medical center near her small town, Gwenie drove over 400 miles to Billings, MT to seek treatment. Like many others who crash into dialysis, she woke up with a CVC catheter on dialysis in the hospital. Upon discharge, Gwenie was sent to her closest dialysis facility for outpatient dialysis, 60 miles away on an Indian reservation. She describes the experience as “the blind leading the blind.” She received no information on home modalities at that clinic, and only learned about her options on the Internet. She approached her clinic about this option.
Gwenie lives on a ranch in a rural area of NE Montana. She is not new to the healthcare arena, but had no idea that she had CKD when she “crashed” into dialysis in Nov. 2020. With no major medical center near her small town, Gwenie drove over 400 miles to Billings, MT to seek treatment. Like many others who crash into dialysis, she woke up with a CVC catheter on dialysis in the hospital. Upon discharge, Gwenie was sent to her closest dialysis facility for outpatient dialysis, 60 miles away on an Indian reservation. She describes the experience as “the blind leading the blind.” She received no information on home modalities at that clinic, and only learned about her options on the Internet. She approached her clinic about this option.
Therein lay the problem. Despite no regulation requiring a care partner for the machine she would be using at home, the clinic required that her husband be in attendance for her entire dialysis training — 3 days a week for 4-6 weeks. Gwenie and her husband operate a working ranch with livestock, so one of them has to be present on the farm at all times. The clinic would make no accommodations for this, so Gwenie did more Internet research. She found a clinic in Fargo, ND that would train her for solo dialysis. So, in the Spring of 2021, Gwenie will relocate 500 miles away to Fargo for 4-5 weeks to begin her training for solo home dialysis.
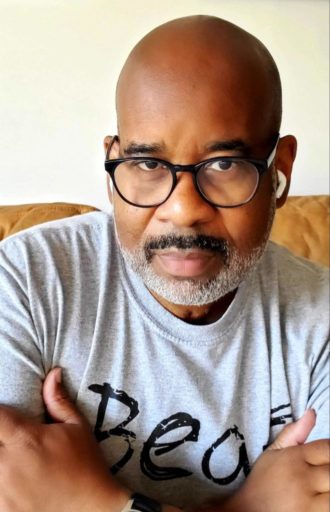
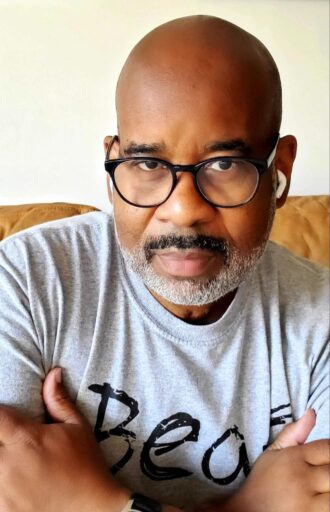
 John recently received a kidney transplant, but he is a veteran of dialysis, experiencing all modalities of treatment. However, when John first made the decision to transition to home hemodialysis (HHD), he found that his options were limited.
John recently received a kidney transplant, but he is a veteran of dialysis, experiencing all modalities of treatment. However, when John first made the decision to transition to home hemodialysis (HHD), he found that his options were limited.
Even though he was in an urban area, he found there were few dialysis centers that offered HHD training. With the assistance of his nephrologist, John was able to identify a center that met his needs, but it was 45 minutes away, and not conveniently located near public transportation. This is a challenge for an individual dependent upon public transportation.
However, John persevered, selected the center, was able to complete his HHD training and experienced great success with HHD.
 Vy is an avid Muay Thai boxer and sandwich blogger living in Orange County, CA. Vy joined a new kidney-specialized care management program 3 weeks after having started in-center hemodialysis. While he had done some of his own research on dialysis, Vy started dialysis without fully understanding all the options. Like many dialysis patients, he did not know about his self-dialysis options.
Vy is an avid Muay Thai boxer and sandwich blogger living in Orange County, CA. Vy joined a new kidney-specialized care management program 3 weeks after having started in-center hemodialysis. While he had done some of his own research on dialysis, Vy started dialysis without fully understanding all the options. Like many dialysis patients, he did not know about his self-dialysis options.
He engaged with his new care team and outlined what his goals were, both for treatment and his lifestyle. It was really important to him to keep up his active lifestyle and get back to Muay Thai boxing 3-4 times a week. After receiving in-depth, customized education on all of his treatment options and talking it through with his dedicated nurse, Vy decided to switch to peritoneal dialysis. This decision allowed Vy to get back to the ring and live his best life.